AMAB-to-neutrois GRS
While nearly anyone who has heard of anything regarding transgender issues has heard of the more “traditional” GRS for AMAB people (used to construct a neovagina and labia from existing penile/scrotal tissues), this procedure does not cover the bases for every AMAB person. In particular, a growing number of non-binary-identified people — in particular, ones with a neutrois identity — are much more interested in simply eschewing their external genitalia entirely.
Although controversial, there are now a few surgeons who will, under the right circumstances, provide this sort of surgery. In January of 2017 I had this procedure done with Dr. Peter Davis in Palo Alto.
Disclaimer
This is a thing that I did because it was right for me, and I knew very well that it was what I needed. I am providing this information as a helpful resource for those who need it. There isn’t any one right way to be trans or nonbinary, and what’s right for me isn’t necessarily right for anyone else.
Updates
2020-04-16: I have added some frequently-asked questions to the FAQ section. Please check that before posting a comment! Thanks.
2020-12-12: Updated the surgeon list.
2021-05-26: Added some updates regarding post-operative care.
2022-09-01: Added some notes on pronouns, cleaned up some awkward phrasing, and updated some stuff regarding my long-term healing.
2022-09-09: Added some information about AFAB-to-neutrois (aka FtN) practitioners.
2023-01-09: As noted in the comments, there’s some pretty big news: WPATH 8 recently released, and this comes with a whole bunch of new guidelines for these surgeries! Hopefully this article will soon be a relic of the past, and general information is much more freely available to all who want it. Thanks to reader WheelyCurious for bringing this to my attention!
Terminology
It is important to describe some of the various terms that are used for these procedures.
- Nullification: the complete or partial removal of a body part (in this case, genitalia)
- Penectomy: the removal of the penis (also sometimes called “phallectomy”)
- Orchiectomy: the removal of the testes
- Clitoroplasty: the construction of a sensate clitoris, usually from the existing glans tissue
- Urethral reroute: directing the urethral opening to a more appropriate location
Dr. Davis offers a procedure, which he at the time called “Nulloplasty,” which refers to the combination of penectomy, orchiectomy, urethral reroute, and a modified clitoroplasty in which a homologous sensate region is formed.
This is related somewhat to the so-called “cosmetic SRS/GRS” that is offered by some of the Thai surgery clinics, also known as a “zero-depth procedure” or a “partial SRS/GRS.” Davis' nulloplasty procedure primarily differs from those procedures in that the clitoris is not exposed (it is buried under the skin, leaving a sensate region) and there is no appearance of labia afterwards.
Other terms I’ve seen for this include “null patch,” “total emasculation,” “smoothie,” and “nullo.” I am fine with the use of “null patch” in regards to me but please do not use the other ones. I also prefer not to use the term “eunuch” in respect to myself, nor do I appreciate any allusions to Barbie or Ken dolls. (Others may be fine with this, of course. It’s all up to the individual.)
Glossary of related terms
- Neutrois: A gender identity that is essentially that of nothing; it is similar to but distinct from “agender” in ways which aren’t worth getting into for this article. (For the Javascript programmers in the audience, the distinction between “neutrois” and “agender” is similar to that between
nullandundefined.) - SRS: Sex Reassignment Surgery (outdated)
- GRS: In newer usage, Genital Reconfiguration Surgery; in older usage, Gender Reassignment Surgery (which is even worse than SRS)
- GCS: Gender Confirmation Surgery (another loaded term that I do not use)
- AMAB: Assigned Male At Birth (generally, someone born with a penis); also referred to as “DMAB” (Designated Male At Birth)
- AFAB: Assigned Female At Birth (generally, someone born with a vulva); also referred to as “DFAB” (Designated Female At Birth)
- ACAB: Not germane to this article
Why I opted for the procedure
This was, of course, a highly personal decision. I consider myself to be transfeminine (or, more broadly, a non-binary trans woman), and while my overall identity varies between feminine-agender and female depending on mood, it is always on the feminine side. However, being asexual, I am not interested in having functional genitalia, and I always liked the aesthetic of a smooth crotch. Long before I’d even heard the word “transgender,” this was what I’d hoped for eventually. While I’d considered the various possibilities of various outcomes, this is the one that always resonated the most with me and seemed the most comfortable.
For many, many years I was trying to find a surgeon who would do what I wanted. There were mumblings in various trans healthcare circles about surgeons who would do it, but they always kept their patients under NDAs because of the controversy around it, especially in the days of the Harry Benjamin standards. I had considered even going with a traditional penile inversion, but it seemed like a lot of expense and necessary aftercare and maintenance for something I was never even going to use anyway, not to mention traditional surgeons' waiting lists were often measured in years.
The 2011 changes to WPATH made more practitioners willing to consider it (especially in mental health circles), but old schools of thought still pervaded the surgical community.
In late 2013 I got tired of waiting and, at least to keep myself partially satisfied (while still being unsure about what I wanted to ultimately do in terms of GRS), I scheduled an orchiectomy in early 2014. This handled the majority of my dysphoria (which was hormonal in nature), but I still had some lingering unhappiness that needed to be addressed. So I continued looking for surgeons who I could work with for the rest of the procedure, but kept on coming up empty-handed.
I did hear about a couple of doctors who would supposedly do the procedure, but they required me to jump through hoops even to schedule a consult with them. For example, one surgeon would only even give me the time of day if I already had all my letters taken care of, and another had a front-of-office staff that was completely unequipped for dealing with non-local patients and couldn’t understand why I might be unable to do a phone-based consultation at the crack of dawn in Central time (and my attempts at finding a better time for the phone consult were all ignored).
I also got in touch with the various Thai clinics that claimed to offer this service, but the information I got back from them showed a distinct lack of knowledgability in terms of what I was looking for, and I got a very bad vibe from them (or at least from their English-speaking representatives). They also claimed an in-hospital recovery time of a month or more, which seemed like an awfully long time to be away from my kitties (not to mention the rest of my life).
As an aside, it was also really frustrating how I looked just feminine enough that there was a roughly 50% chance that TSA screeners at the airport would push the pink button when I walked through the x-ray, which would of course flag my penis, which would then lead to a rather frustrating experience where the two screeners would argue about who had to grope me (i.e. whether I was male or female) without ever thinking to ask me, the human being standing right in front of them. Personally I didn’t care — I just wanted the groping to get over with. Or to not happen at all.
A brief history of nullification
Historically, eunuchs have been the keepers of harems, and were often selected from those who were intersex or transgender. This was often a very brutal practice; in China, for example, they would simply have their penis and testes removed with a knife and have a feather put into the urethral opening to prevent it from closing up. There was a high risk of infection and death.
In the late 20th century, similar practices were performed in the extreme body modification community, often for fetishistic purposes. This would be documented on the down-low on sites such as eunuch.org and BME (both links NSFW), and a lot of the information was generally poor-quality or pure fiction presented as legitimate medical information.
The rare times a surgeon would offer this procedure, it wasn’t done much more thoughtfully than the Chinese eunuch technique; the knife would be sterile and the feather would be a stent, and the suspensory ligaments would be severed to allow the urethral opening to drop naturally, but the rates of strictures were high and the surgeons involved tended to not see it as a legitimate medical treatment – they’d do the procedure as quickly as possible and then look the other way, often even putting the patient under an NDA.
Enter Dr. Peter Davis
In mid-2016, I heard from my primary care doctor (who specializes in LGBT+ healthcare) that she’d just heard about Peter Davis, a surgeon who would do what I wanted, and that one of her other patients had this procedure done. I was elated!
So, as soon as I could, I called Dr. Davis and scheduled a consult. He was very excited to talk about the procedure, and also compare it to the other surgeons' approaches. He also got me in touch with the other local patient, who I met up with for coffee and was able to get a really good idea of how things would go.
Dr. Davis takes a very different approach to this surgery. Rather than see it as a thing to wash his hands of as soon as possible, he sees it as just another variation on more traditional GRS procedures. As a result, he’s also gotten several male-identified people who want the procedure done as part of their sexual identity (rather than gender identity) – such as the person who told my doctor about him in the first place. (Frustratingly, much of the new-school medical literature around this surgery revolves around that particular identity, which leads to a different sort of erasure and misinterpretation, but at least the procedure is becoming available!)
This does lead to my only gripe with Dr. Davis; at the time of my procedure, he had a difficult time with pronouns and with the idea that there are multiple sorts of identities that have the same end result in surgery. In my case he kept on referring to me with female pronouns, which was okay but not ideal (at the time my preference was they/them and he expressed an inability to adjust to using “singular they,” although at least he was respectful about it being a problem on his end and not with me), but apparently several male-identified patients got the same “she/her” treatment from him as well.
At least as of late 2016 his waiting list was very short; I had the initial consult in November, and in December I had the surgery scheduled for January 2017.
The procedure
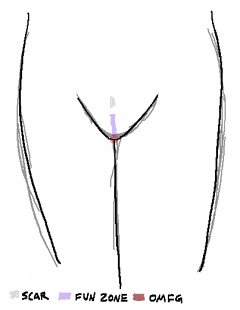
Davis' procedure treats nullification similarly to a penile inversion procedure wherever possible, with a few (obvious) modifications. One of the things he prides himself on – which I am very happy for him to have done – is in maintaining as much sensitivity as possible, and forming a pseudoclitoris that is buried under the skin. Most of the time spent in surgery is him very carefully excising and routing the nerves, which is incredibly delicate (and would not be so necessary with penile inversion, where the nerves would have remained affixed to skin which is not retained in this procedure). The end result of this is that I have a sensate region (or, as Dr. Davis calls it, a “fun zone”) in the area in front of my urethra; there is also still a bit of erectile tissue but this isn’t bothersome to me at all.
Another thing he does is to reshape the pubis mons to make it match up better with the contours of the surrounding tissue.
For the most part, the surgery leaves everything the way it would be for a more “standard” MTF procedure; it’s just that the resulting shape is as if the tissue were undifferentiated and smoothed down.
Other surgeons' procedures also increase the chance of a urinary stricture; while any surgery involving the urethra can lead to a stricture, Davis prides himself on having never had a patient develop one (and he has also helped patients of other surgeons to clear up their strictures as well).
Recovery
Initial post-op
The staff at the hospital was pretty abysmal. They rushed me through recovery (outpatient!) and didn’t even attempt to respect my gender (calling me “he” even though I was recovering from GRS, and despite my repeated pleading otherwise!) or basic comfort. I ended up complaining to the hospital administration afterwards and they said they would address this.
After discharge, I spent the next several days at a friend’s home in San Francisco. He went above and beyond in taking care of me after the procedure, although most of the time I just slept and took painkillers. (My recommendation: if you have access to cannabis products, take advantage of it. They helped me out both in terms of pain management and in keeping my brain occupied.)
During the surgery, Dr. Davis put in a nerve block which lasted a few days, keeping me quite numb for a while. This felt vaguely annoying, but as soon as it wore off, I wished I could have another one for a while. I wouldn’t say it was the worst pain in my life, but it certainly wasn’t particularly pleasant. Most of the pain was really from the catheter, which Dr. Davis had sewn in place to keep it from falling out. The catheter also made it feel like I needed to pee all the time (although I suppose that technically I was peeing all the time, so).
I had the surgery on Thursday, and my followup – getting the catheter removed – was on Monday. After that I learned very quickly that one really should get a bunch of maxi-pads for this procedure as well; part of the procedure involves removing/severing pretty much all of the bladder muscles, so there was a pretty constant drip of urine. Which was, of course, not particularly pleasant for myself or for those around me.
UPDATE: From what I’ve heard, Dr. Davis has updated his procedure to not require severing the pelvic/bladder muscles, so this is probably less of an issue now.
Come to think of it, here are the things nobody told me but which I found out soon enough anyway:
- The numbness is normal, and is from the anaesthesia block. It only delays the inevitable.
- There will be itching. Lots of itching. In places that cannot be scratched. Because they no longer exist.
- Some of the sutures will poke out and grab at anything nearby. Some of the pokey bits will be right by the urethra. Do not be alarmed. (You will be alarmed.)
- Average response to oxycodone is just an average. You might be significantly more receptive to it. You might be significantly less receptive to it. If you’re lucky you might only need to take half a pill a couple times a day for a few days and have no withdrawal. I was not lucky.
- And speaking of which, not only do you really want to take the stool softener regularly while you’re on oxy, you’ll really want to drink as much water as you can, too — otherwise the stool softener doesn’t actually do anything useful, and can even end up making this worse.
- You will need maxi-pads. Lots of maxi-pads. Do not get the thin ones. Get the thickest, softest, heaviest-flow ones you can find. However you will not be in any state for going to the store yourself when you need them, so either buy them ahead of time or get VERY specific with whomever is taking care of you. (If it’s a dude, make sure they know the difference between tampons and maxi-pads first.) Expect to use three a day for a while, at the very minimum.
- Kegels. Right now. Do sets of them whenever you have a moment. Even if you think you aren’t going to ever, ever do this in a million years, do your Kegels. Even if this article doesn’t even apply to you. Kegels. They’re great™.
- Skirts are comfortable af to lounge around in
Bob Ross is on NetflixUPDATE: Sadly, no longer true 😞
Post-surgery travel and beyond
It’s a pretty good idea to arrange to be wheeled around the airport. I didn’t, figuring I could get assistance while at the airport. That ended up not being so simple. Unfortunately, at the time, my airline of choice (Alaska) flew out of SFO’s international terminal, which doesn’t have the same accommodations as the domestic terminal, and the walkways are long. So I took it really, really slow. Alaska Airlines was nice enough to allow me to preboard, and also offered assistance on the jetway (which I should have taken, but I didn’t, stubborn fool that I am) and my simple refusals to get sufficient help probably set my healing back quite a bit.
In fact, I did develop a pretty nasty complication from all this – granulation tissue. I would not recommend doing an image search on that, because it looks pretty nasty; basically, if you’ve ever skinned your knee, and have developed painful crystal-looking scab whatever gross stuff on the skin afterwards? That’s granulation tissue. In my case it was up in my urethra, which made a lot of stuff (sitting, standing, walking, peeing, doing nothing at all, etc.) rather painful at times. It took a few weeks to clear up.
Oh, and while my recovery from the orchiectomy was easy and straightforward and I hardly had to take painkillers at all, this time things were persistently painful for long enough that I had to take them for a couple weeks. Fortunately, Dr. Davis prescribed me some anti-nausea medications “just in case you need it” but not saying when I might need them. They were for the oxycodone withdrawal, as it turns out. (And very, very helpful at that.)
I also developed an infection! Because I was remiss in actually using the tube of bacitracin gel that the hospital provided me. So, I ended up taking a course of antibiotics for that. Which then wiped out my intestinal flora, which led to some very, very unpleasant times on the toilet. Which hurt to use, because of the granulation tissue. (The worst of the toilet problems at least cleared up with some probiotics.)
The granulation tissue was especially difficult while walking (which I enjoy doing a lot of) and sitting on the hard chairs at the coffee shops I like to work at. Probably the worst part of recovery was this long-term restlessness from having to seriously adjust my daily work routines and not being able to spend as much time socializing as before.
All in all I’d put my total recovery at about two months before I was feeling reasonable, and another month before I felt normal.
Oh, but what a feeling it was.
The new normal
It didn’t take my brain very long to adjust to the new sensory mapping. It’s almost as if this is the way I was supposed to be configured to begin with! Go figure.
I still have a few weird moments where I’m expecting something to hit me in the dick, and there’s no dick in which to be hit. But that’s just kind of giddy-inducing to me. It’s not unlike the feeling of having a haircut for the first time in two years.
Very rarely I’ll get phantom nerve sensations, like a deep, firey-cold itching that I can’t scratch (at least, not in public, because of where it is). It usually passes in a couple minutes, and while it happened a lot throughout February (which was the primary inspiration for a game I made that month) it’s pretty infrequent at this point and only lasts a few seconds.
While orgasm isn’t a high priority for me, I did finally figure out how to do it again, using a vibrator. This is something that takes some experimentation and is probably very personal.
There is a bit of a scar where the base of my penis was, but that’s healing and has faded somewhat over time. It’s not very visible, although it’s easy to feel. It’s totally covered over by my pubic hair, at least. The scar itself is numb on the surface, as is the incision line beneath it; however, this doesn’t really affect anything in the day-to-day experience of being me. It does add a bit of a “wrinkle” to my pubis mons, however.
There was also a very slight visible bump over my pseudoclitoral sensate region. It has the look and feel of loose skin more than anything else, although that has mostly faded.
I do sometimes think that perhaps I should have done a zero-depth/“cosmetic”/partial GRS instead, although I’m not unhappy with my results. It’s easy to second-guess decisions but regardless of other possibilities, I am totally happy with what I have now.
I’m also finding myself wearing distinctly feminine clothing a lot more lately. It just seems more comfortable to me now, and I’ve had a much stronger desire to express my internal gender outwardly.
Meanwhile, I’ve been trying to come up with a pithy term for what to call my configuration. The best I’ve got is that I used to have junk but now I’ve been decluttered.
I no longer get groped by the TSA.
Administrativa
Not everything went totally smoothly (so to speak)! While the surgery itself was great, there were some complicating factors external to it.
Insurance coverage
My insurance claimed to cover transgender surgery at 80%. There is fine print, however: it is “80%, up to the allowable limit,” and their idea of “allowable limit” is bafflingly low (as in, around $5000). Between that and my deductible, insurance didn’t really cover the surgery to any meaningful degree. However, it did cover a lot of the hospital expenses, so it’s a good idea to go in-network for the hospital itself.
However, if you do go with insurance up front, the cost of the surgery will be even higher, so unless Dr. Davis is in-network (he probably isn’t) and your allowable limit exceeds his price (it probably won’t) you’ll probably want to go out-of-pocket and get reimbursed. If you do that, make sure that you get an itemized bill that includes, for every procedure:
- Diagnostic code and name
- Procedure code and name
and the bill itself needs to include the tax ID as well. This will make dealing with insurance much easier. I had difficulty getting this information from Dr. Davis' office. Hopefully this is something they’ve gotten better at since then.
Recommendation letters
WPATH guidance calls for two letters of recommendation from mental health providers, with some specific restrictions on the sorts of credentials. At least when I scheduled with Dr. Davis, he worked with a preferred psychologist who would write letters for him. While she served the purpose of getting my second letter written, I would not recommend her for those who have another option available; she had some serious issues with respecting my identity, not to mention her personal organization, sending the right letter to the right person and the right mailing address, taking payment, not casually violating HIPAA, and so on.
Scheduling
I would also highly recommend doing stuff as far in advance as possible with Dr. Davis; his office staff are fairly disorganized and there were some very close calls in terms of me getting my required information, settling payment, scheduling the work, and so on. As his practice grows I hope he gets these kinks worked out, because they were black marks on an otherwise excellent experience.
Known practitioners
In addition to Dr. Davis, there are a few other surgeons who perform at least some variation on nullification. I cannot speak to their quality or procedure.
- Dr. Thomas Satterwhite in San Francisco
- Dr. Curtis Crane in San Francisco
- Dr. Loren Schechter in Chicago
- Dr. Daniel Dugi in Portland, OR
- Dr. Tuan A. Nguyen in Lake Oswego, OR (this one came with a positive recommendation from a prior patient)
- Mozaic Care in San Francisco offers an extremely wide variety of gender-nonconforming GRS options
I have also been told that Dr. Marc Arnkoff of Michigan should be extremely avoided; the personal testimonial I got regarding his procedure was extremely negative in ways that I would never want anyone to be subjected to.
Questions I’ve been asked
Here are some frequently-asked questions.
What are the correct pronouns for someone who’s undergone this procedure?
Pronouns are not determined by genital configuration. If you want to know someone’s pronouns, ask them.
Mine, incidentally, are she/her or they/them.
How hard was it to find practitioners?
This was pretty difficult in the past, but things have gotten a lot better now. Surgeons in general still have great difficulty with this, but there are practitioners like Dr. Davis who are coming around. The general difficulty has mostly been with general practitioners, therapists, and so on, but that’s definitely gotten a lot better with the improved visibility of nonbinary/trans identities in general. Also I had trouble with my prior doctors and certain mental health professionals I’ve worked with. But fortunately, Seattle is really good for transgender stuff, and I’ve been very happy with my current therapist and doctor, and of course Dr. Davis was on the whole really good about this (aside from the pronoun issue).
The approval letters are the more difficult thing. I can offer suggestions for therapists in both Seattle and San Francisco, but as far as the PhD requirement (as specified by WPATH) it’s somewhat more difficult to find letter-writing psychologists.
How informed were you going in?
The discussions with Dr. Davis were very, very informative about what the procedure would entail, and it had also matched my expectations based on having read up on the various forms of surgery that have existed throughout the years. My main concern was about the preservation of sensitivity, but that ended up being the main thing he focused on in our discussions, and he was especially proud of the techniques he developed for preserving the nerve endings in the sensate region.
By the time I finally got this to happen I was just so freaking relieved to finally be getting it taken care of. I will say that I was really anxious for my orchiectomy (and even had a panic attack that was so bad the surgeon nearly canceled it on me!) but for the nullification? I couldn’t get on the operating table fast enough.
How did it feel afterwards? Better, worse, foreign?
This was a change I wanted and needed and was going into specifically to get rid of the feelings I didn’t like. While there was a fairly short period of adjustment to a new sensory mapping, it all felt good and right to me. Of course there was a slight adjustment period but it was all in service of a change I wanted, which makes a huge difference.
Obviously this is just what was right for me though! See again my disclaimer at the top – this was the decision I felt was best for me and there is no one right way to be transgender or agender or neutrois or whatever. If you don’t feel that you need this, don’t do it! It won’t actually improve your life in any way outside of eliminating physical dysphoria; so, unless you already feel like you need this, don’t take this article as inspiration for doing it.
Why would you do this? Why would anyone do this?
I 100% did this for myself. It’s probably easier for me to make that decision being asexual in the first place, but even if you are a sexual being, if this is the sort of thing you’d want to do, then it’s your body and your decision. There is nothing about this procedure that makes any real impediment to sex, although you might need to get a bit more creative.
Also, my experience in talking about this with people who have no investment has led me to realize that most people who give a crap about how your body is configured are going into it from a perspective of entitlement. Why should I care if someone I wasn’t going to have sex with anyway doesn’t want to have sex with me even more now?
Your body is your own, and the way you decide to have relations with others is your choice. If someone cares about you, they’ll adjust. If they refuse to adjust, it’s their problem, not yours.
Is there any similar procedure for AFAB people?
I have no idea! I’d hope so, but unfortunately, whereas the procedure as applied to AMAB folks is highly controversial, I’d expect the AFAB equivalent to fall under the umbrella of female genital mutilation. As usual, female-designated bodies being way more strongly policed than male-designated bodies. You can probably find someone who will do it but I wouldn’t know where to begin.
One approach I can think of – and again, keep in mind that this isn’t something I’ve had to seriously look into – is to look for a surgeon who will do a metoidioplasty and vaginectomy, and see if they’ll do a similar clitoral burial as what Dr. Davis did for me. And if you do get information on this, please consider writing an article like this one – it never hurts to have more information available for those who need it!
Update: I have heard that both Mozaic Care and The Crane Center have an AFAB nullification (FtN) procedure available as well. Again, I am in no way qualified to comment on their procedures, but I hope this is a helpful starting point for a search.
What about other atypical GRS procedures?
I know of others who have done pretty much the opposite from me – having a penis-preserving vaginoplasty, for example. It’s getting at least somewhat visible and available now, and Mozaic Care in San Francisco advertises gender-non-conforming GRS services. I haven’t worked with them and don’t know anyone who has, but they are certainly someone to talk to if you have something in mind!
What did it cost?
The surgery itself cost US$10,000, and there were additional hospital fees as well, most of which were covered by my insurance. Prices will have gone up since then and it’s hard to predict what the hospital fees will be because of the quagmire that is the US health insurance industry. I was able to get a partial reimbursement from my insurance and my total out-of-pocket expense was around US$13,000 when all was said and done.
This will vary quite a lot based on your own insurance situation.
Is electrolysis necessary for this like it is with most vaginoplasty procedures?
Nope! The purpose of electrolysis in a vaginoplasty is to prevent having active hair follicles which grow into the vaginal canal and the inner folds of the labia. As those parts do not exist with this procedure, no electrolysis is necessary.
Update: (2021/05/26) That said, I would recommend getting some amount of electrolysis around where the urethral opening will be, if you’re comfortable with that; I find that some of my hair grows in uncomfortably close to my urethral opening and it’s quite sensitive to pluck it. (I happen to enjoy it, but it’d definitely not be for everyone!)
If I get an orchiectomy before this, do I need to preserve the scrotal tissue?
I don’t believe so. I had preserved mine simply because I wasn’t sure if I was going to go with this procedure or a typical GRS, but as far as I can tell none of that was kept for the final result.
What’s aftercare like?
Wearing tighter-than-usual underpants to keep pressure applied to the surgery site, keep it clean, use vitamin E lotion, don’t push yourself physically.
Could a version of this limit all sexual desire/libido? Could I get this done without the buried clitoris?
So, libido is a complex subject which I am absolutely not qualified to talk about, but in extremely broad terms, libido lives in the brain, not in the genitals. It’s affected by the hormones which are produced by the gonads, and so an orchitectomy or an oophrectomy can reduce (but not eliminate) one’s libido, but in general, if you have an antagonistic relationship with your libido, the appropriate first-line course of treatment is therapy, not surgery.
With all that said:
My libido hasn’t been greatly affected by this procedure itself; what little libido I did have before was pretty much made irrelevant by my previous orchiectomy.
I am able to bring myself to orgasm if I need to, but it’s rare that I need to. I do appreciate being able to, though. For this reason I do recommend keeping the buried clitoris; for starters, having it apparently greatly reduces the recovery time in terms of reducing phantom nerve sensations (after all, it’s easier to retrain the brain about nerve endings moving around than it is about them being entirely gone), but also it’s easier to have a thing and not use it than it is to not have a thing that you do need to use.
From what I’ve heard from people who have had non-sensory-preserving procedures done, it’s still possible to orgasm with much greater difficulty, but the ongoing frustration of being unable to achieve any sort of sexual release when it’s necessary would, to me, not be worth it.
Do you know anyone else who has done this?
Several people, now, many of which learned of this procedure from this very article. I should start charging a finder’s fee.
Can you share actual recovery/result pictures?
I can provide access to some, yes, although for what should be obvious reasons I don’t want to provide them to just anyone. If you sign in at this link you can request access to the entry there, or if that doesn’t work you can let me know (via email, Mastodon, etc.) who you are (including the identity you used to log in) and why you want to see them, I may grant you access at my discretion.



Comments
Before commenting, please read the comment policy.
Avatars provided via Libravatar